-
Functional Areas
- Principal Recipient Start-Up
-
Legal Framework
- Overview
- Project Document
-
The Grant Agreement
- UNDP-Global Fund Grant Regulations
- Grant Confirmation
- Grant Confirmation: Face Sheet
- Grant Confirmation: Conditions
- Grant Confirmation: Conditions Precedent (CP)
- Grant Confirmation: Special Conditions (SCs)
- Grant Confirmation: Schedule 1, Integrated Grant Description
- Grant Confirmation: Schedule 1, Performance Framework
- Grant Confirmation: Schedule 1, Summary Budget
- Implementation Letters and Performance Letters
- Agreements with Sub-recipients
- Agreements with Sub-sub-recipients
- Signing Legal Agreements and Requests for Disbursement
- Language of the Grant Agreement and other Legal Instruments
- Amending Legal Agreements
- Other Legal and Implementation Considerations
- Legal Framework for Other UNDP Support Roles
-
Health Product Management
- Overview - Health Product Management
- UNDP Quality Assurance Policy
- Product Selection
- Quantification and Forecasting
- Supply Planning of Health Products
-
Sourcing and regulatory aspects
- Global Health Procurement Center (GHPC)
- Development of List of Health Products
- Development of the Health Procurement Action Plan (HPAP)
- Health Procurement Architecture
- Local Procurement of health products
- Procurement of Pharmaceutical Products
- Procurement of non-pharmaceutical Health Products
- Other Elements of the UNDP Procurement Architecture
- Submission of GHPC CO Procurement Request Form
- Guidance on donations of health products
- International freight, transit requirements and use of INCOTERMS
- Inspection and Receipt
- Storage
- Inventory Management
- Distribution
- Quality monitoring of health products
- Waste management
- Rational use
- Pharmacovigilance
- Risk Management for PSM of health products
- Compliance with the Global Fund requirements
- UNDP Health PSM Roster
-
Financial Management
- Overview
- Grant-Making and Signing
- Grant Implementation
- Sub-recipient Management
- Grant Reporting
- Grant Closure
- CCM Funding
- Import duties and VAT / sales tax
-
Monitoring and Evaluation
- Overview
- Differentiation Approach
- Monitoring and Evaluation Components of Funding Request
- Monitoring and Evaluation Components of Grant Making
- M&E Components of Grant Implementation
- Sub-Recipient Management
- Grant Reporting
-
Capacity development and transition, strengthening systems for health
- Overview
- Interim Principal Recipient of Global Fund Grants
- A Strategic Approach to Capacity Development
- Resilience and Sustainability
- Legal and Policy Enabling Environment
- Functional Capacities
- Capacity Development and Transition
- Transition
- Capacity Development Objectives and Transition Milestones
- Capacity Development Results - Evidence From Country Experiences
- Capacity development and Transition Planning Process
- Capacity Development and Transition - Lessons Learned
-
Risk Management
- Overview
- Introduction to Risk Management
-
Risk Management in the Global Fund
- Global Fund Risk Management Framework
- Local Fund Agent
- Challenging Operating Environment (COE) Policy
- Additional Safeguard Policy
- Global Fund Risk Management Requirements for PRs
- Global Fund Risk Management Requirements During Funding Request
- Global Fund Review of Risk Management During Grant Implementation
- Risk management in UNDP
- Risk Management in UNDP-managed Global Fund projects
- UNDP Risk Management Process
- Risk management in crisis settings
- Audit and Investigations
- Human rights, key populations and gender
- Human resources
-
Grant closure
- Overview
- Terminology and Scenarios for Grant Closure Process
-
Steps of Grant Closure Process
- 1. Global Fund Notification Letter 'Guidance on Grant Closure'
- 2. Preparation and Submission of Grant Close-Out Plan and Budget
- 3. Global Fund Approval of Grant Close-Out Plan
- 4. Implementation of Close-Out Plan and Completion of Final Global Fund Requirements (Grant Closure Period)
- 5. Operational Closure of Project
- 6. Financial Closure of Project
- 7. Documentation of Grant Closure with Global Fund Grant Closure Letter
Human Rights
Evidence shows that human rights barriers can impede the access to and uptake of critical HIV, TB and malaria prevention, treatment and care services. In the context of HIV, these barriers can include punitive legal or policy environments that criminalize, or otherwise punish, key populations; widespread stigma and discrimination; and lack of informed consent or medical confidentiality. High levels of human rights violations and discrimination against members of key populations increase their vulnerability to HIV and deter access to HIV prevention, treatment, care and support services. Laws that criminalize or otherwise punish the behaviour of key populations, as in the case of men who have sex with men (MSM), male/female/transgender sex workers (SW), people who use drugs (PWUD), or transgender people, present additional barriers to access to services.
People in prison, or other closed settings, can also be negatively impacted by punitive norms that hinder their access to services (e.g., gender insensitive conditions, ban on harm reduction services, lack of access to condoms and Pre-exposure prophylaxis (PrEP)). People living with TB —a disease associated with poverty and social inequality that particularly affects vulnerable populations with poor access to basic services— can experience high levels of stigma and discrimination or unnecessary and mandatory hospitalization that deviates from the WHO guidelines, unavailability of TB prevention and treatment services in prisons, or lack of access to TB services (for instance, for migrant workers).
Less is known about the intersection of human rights and malaria. However, malaria is also linked to poverty, with migrants, refugees, rural populations, prisoners, and indigenous populations experiencing high rates of infection. Social inequality and political marginalization may impede access to health services, and additional barriers may be created by language, culture, poor sanitation lack of access to health information, lack of informed consent in testing and treatment, and inability to pay for medical services.
Table 1: The table below highlights the possible legal and policy environment’s impact on the number of people infected with HIV.
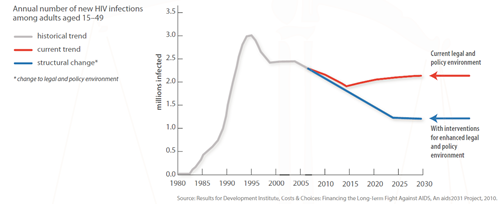
This fact sheet includes examples of how laws and practices can obstruct the HIV response and waste resources for support treatment and prevention efforts, as well as potential positive outcomes when good practices and laws based on human rights and available evidence are enforced.
Promoting and protecting rights in the context of HIV and TB is critical to ensuring that investments in national responses are fully realized.
Author: Global Commission on HIV and the Law Language: English Type: Policies, procedures and guidance Topic: Human rights and the law
Author: Global Commission on HIV and the Law Language: English Type: Policies, procedures and guidance Topic: Human rights and the law