-
Functional Areas
- Audit and Investigations
-
Capacity development and transition, strengthening systems for health
- A Strategic Approach to Capacity Development
- Capacity Development and Transition - Lessons Learned
- Capacity development and Transition Planning Process
- Capacity Development and Transition
- Capacity Development Objectives and Transition Milestones
- Capacity Development Results - Evidence From Country Experiences
- Functional Capacities
- Interim Principal Recipient of Global Fund Grants
- Legal and Policy Enabling Environment
- Overview
- Resilience and Sustainability
- Transition
-
Financial Management
- CCM Funding
- Grant Closure
- Grant Implementation
- Grant-Making and Signing
- Grant Reporting
- Import duties and VAT / sales tax
- Overview
- Sub-recipient Management
-
Grant closure
- Overview
-
Steps of Grant Closure Process
- 1. Global Fund Notification Letter 'Guidance on Grant Closure'
- 2. Preparation and Submission of Grant Close-Out Plan and Budget
- 3. Global Fund Approval of Grant Close-Out Plan
- 4. Implementation of Close-Out Plan and Completion of Final Global Fund Requirements (Grant Closure Period)
- 5. Operational Closure of Project
- 6. Financial Closure of Project
- 7. Documentation of Grant Closure with Global Fund Grant Closure Letter
- Terminology and Scenarios for Grant Closure Process
- Human resources
- Human rights, key populations and gender
-
Legal Framework
- Agreements with Sub-recipients
- Agreements with Sub-sub-recipients
- Amending Legal Agreements
- Implementation Letters and Performance Letters
- Language of the Grant Agreement and other Legal Instruments
- Legal Framework for Other UNDP Support Roles
- Other Legal and Implementation Considerations
- Overview
- Project Document
- Signing Legal Agreements and Requests for Disbursement
-
The Grant Agreement
- Grant Confirmation: Conditions Precedent (CP)
- Grant Confirmation: Conditions
- Grant Confirmation: Face Sheet
- Grant Confirmation: Schedule 1, Integrated Grant Description
- Grant Confirmation: Schedule 1, Performance Framework
- Grant Confirmation: Schedule 1, Summary Budget
- Grant Confirmation: Special Conditions (SCs)
- Grant Confirmation
- UNDP-Global Fund Grant Regulations
-
Monitoring and Evaluation
- Differentiation Approach
- Monitoring and Evaluation Components of Funding Request
- M&E Components of Grant Implementation
- Monitoring and Evaluation Components of Grant Making
- Overview
- Principal Recipient Start-Up
-
Health Product Management
- Compliance with the Global Fund requirements
- Distribution
- Inspection and Receipt
- International freight, transit requirements and use of INCOTERMS
- Inventory Management
- Overview
- Pharmacovigilance
- Product Selection
- Quality monitoring of health products
- Quantification and Forecasting
- Rational use
- Risk Management for PSM of health products
-
Sourcing and regulatory aspects
- Development of List of Health Products
- Development of the Health Procurement Action Plan (HPAP)
- Guidance on donations of health products
- Health Procurement Architecture
- Local Procurement of health products
- Other Elements of the UNDP Procurement Architecture
- Procurement of non-pharmaceutical Health Products
- Procurement of Pharmaceutical Products
- Submission of GHSC CO Procurement Request Form
- Storage
- Supply Planning of Health Products
- UNDP Health PSM Roster
- Waste management
- Grant Reporting
-
Risk Management
- Introduction to Risk Management
- Overview
- Risk management in crisis settings
-
Risk Management in the Global Fund
- Additional Safeguard Policy
- Challenging Operating Environment (COE) Policy
- Global Fund Review of Risk Management During Grant Implementation
- Global Fund Risk Management Framework
- Global Fund Risk Management Requirements During Funding Request
- Global Fund Risk Management Requirements for PRs
- Local Fund Agent
- Risk management in UNDP
- Risk Management in UNDP-managed Global Fund projects
- UNDP Risk Management Process
- Sub-Recipient Management
Human Rights
Evidence shows that human rights barriers can impede the access to and uptake of critical HIV, TB and malaria prevention, treatment and care services. In the context of HIV, these barriers can include punitive legal or policy environments that criminalize, or otherwise punish, key populations; widespread stigma and discrimination; and lack of informed consent or medical confidentiality. High levels of human rights violations and discrimination against members of key populations increase their vulnerability to HIV and deter access to HIV prevention, treatment, care and support services. Laws that criminalize or otherwise punish the behaviour of key populations, as in the case of men who have sex with men (MSM), male/female/transgender sex workers (SW), people who use drugs (PWUD), or transgender people, present additional barriers to access to services.
People in prison, or other closed settings, can also be negatively impacted by punitive norms that hinder their access to services (e.g., gender insensitive conditions, ban on harm reduction services, lack of access to condoms and Pre-exposure prophylaxis (PrEP). People living with TB —a disease associated with poverty and social inequality that particularly affects vulnerable populations with poor access to basic services— can experience high levels of stigma and discrimination or unnecessary and mandatory hospitalization that deviates from the WHO guidelines, unavailability of TB prevention and treatment services in prisons, or lack of access to TB services (for instance, for migrant workers).
Less is known about the intersection of human rights and malaria. However, malaria is also linked to poverty, with migrants, refugees, rural populations, prisoners, and indigenous populations experiencing high rates of infection. Social inequality and political marginalization may impede access to health services, and additional barriers may be created by language, culture, poor sanitation lack of access to health information, lack of informed consent in testing and treatment, and inability to pay for medical services.
Table 1: The table below highlights the possible legal and policy environment’s impact on the number of people infected with HIV.
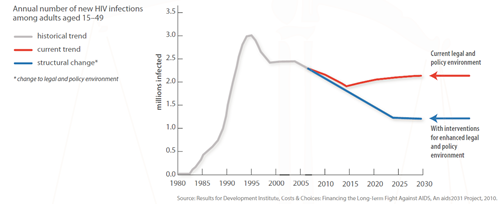
This fact sheet includes examples of how laws and practices can obstruct the HIV response and waste resources for support treatment and prevention efforts, as well as potential positive outcomes when good practices and laws based on human rights and available evidence are enforced.
Promoting and protecting rights in the context of HIV and TB is critical to ensuring that investments in national responses are fully realized.
Loading resources